Mastering Follow-Up ICD-10 Codes: A Comprehensive Guide for Accurate Medical Billing & Compliance
January 4, 2026
ICD-10 Codes Explained: A Practical Reference for Healthcare Providers and Coders
January 4, 2026Assigning the correct ICD-10 code for leukocytosis is a common yet persistent challenge for medical coders, billers, and healthcare providers. Frustrations often arise from clinical ambiguity, where a lab report shows an elevated white blood cell (WBC) count but the documentation lacks the specificity needed for a precise code. This ambiguity is not just an administrative hurdle; it carries the heavy risk of claim denials, reduced reimbursement, and potential audit scrutiny, all of which can strain the financial health of a healthcare organization.
Precision in medical coding for conditions like leukocytosis is fundamental. It ensures that patient records accurately reflect clinical findings, supporting high-quality care and seamless communication between providers. Furthermore, accurate coding is the backbone of a healthy revenue cycle, ensuring that facilities are fairly compensated for the complexity of the cases they manage.
Leukocytosis is a frequent clinical finding, often appearing as a transient response to infection, inflammation, or stress. While the code D72.829, “Elevated white blood cell count, unspecified,” exists to capture these instances, its use requires careful consideration. Using an unspecified code when more detailed information is available can lead to “undercoding,” which may trigger payer rejections or mask the true severity of a patient’s condition. This guide will explore how to navigate these complexities, from understanding the nuances of D72.829 to identifying when more specific codes are required for compliant and accurate billing.
Understanding Leukocytosis in the Clinical and Coding Context
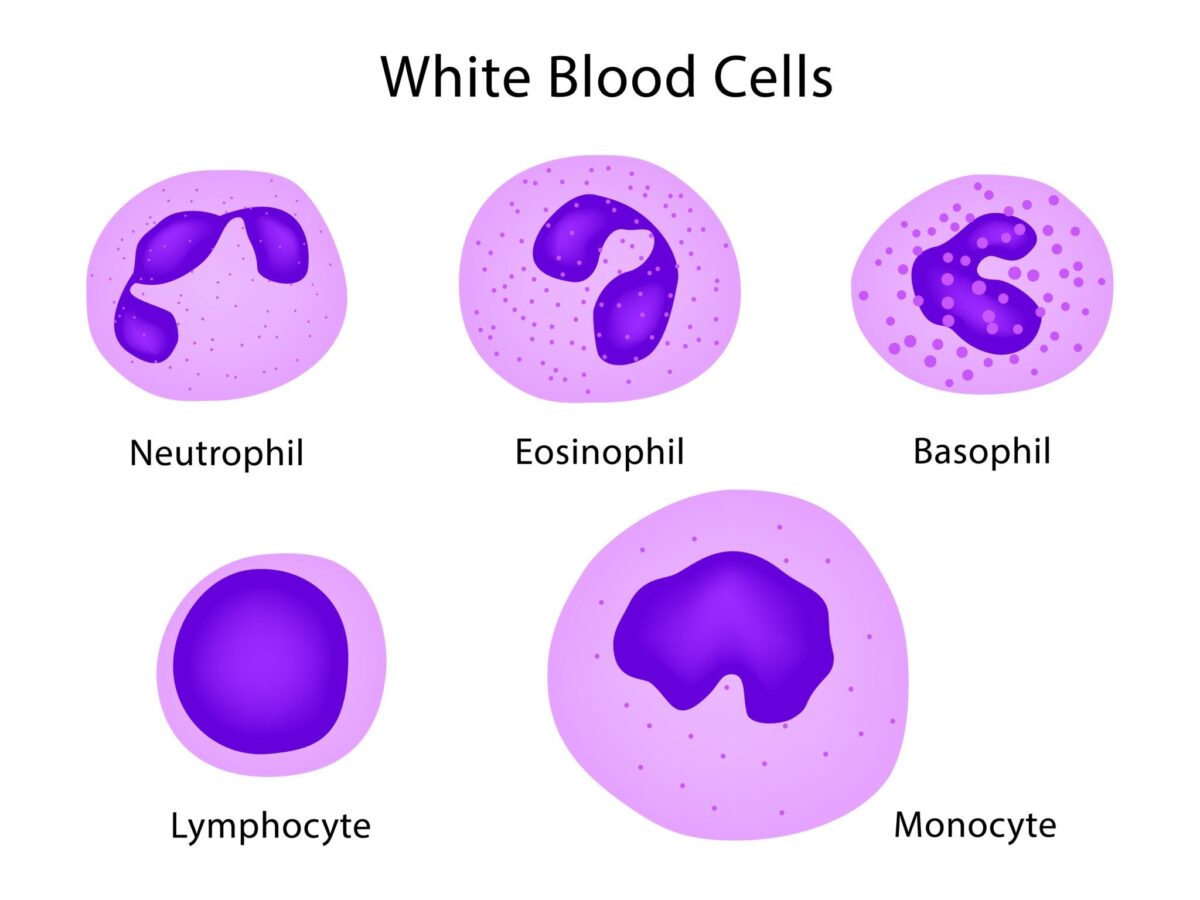
Leukocytosis is defined as an increase in the total number of white blood cells circulating in the blood, typically exceeding the normal upper limit of approximately 11,000 cells per microliter. In the clinical setting, this elevation is a key indicator that the body is responding to an internal or external stimulus. White blood cells are the primary defenders of the immune system, and their proliferation often signals an active battle against a threat.
Common Clinical Causes of Elevated WBC
The reasons for an elevated WBC count are vast and varied, ranging from benign physiological responses to severe, life-threatening pathologies.
- Infections: This is the most common cause, with bacterial, viral, fungal, and parasitic infections all capable of triggering a significant rise in WBCs.
- Inflammation: Chronic inflammatory conditions, such as rheumatoid arthritis or inflammatory bowel disease, can lead to persistent leukocytosis.
- Stress Responses: Physical stress from surgery, trauma, or even severe emotional stress can cause a “stress leukocytosis” as the body releases stored white cells into the bloodstream.
- Medications: Certain drugs, particularly corticosteroids like prednisone, are well-known to increase white blood cell counts.
- Malignancies: Bone marrow disorders and leukemias can cause extreme elevations in WBCs, though these are typically coded under different, more specific ICD-10 chapters.
The Role of D72.829 in Documentation
In the ICD-10-CM hierarchy, D72.829 serves as the “default” code for leukocytosis when the documentation does not provide enough detail to select a more specific subcategory. It falls under Chapter 3: Diseases of the Blood and Blood-forming Organs. Specifically, it is categorized under “Other disorders of white blood cells” (D72) and the subcategory “Elevated white blood cell count” (D72.82).
While D72.829 is a billable and valid code, its use should be reserved for cases where the specific type of white blood cell that is elevated—such as neutrophils, lymphocytes, or monocytes—has not been identified or documented by the provider. As soon as a differential count is available and the provider specifies the type of leukocytosis, a more precise code must be used to ensure coding compliance and accuracy.
Decoding D72.829: When and How to Use It
The code D72.829 is officially described as “Elevated white blood cell count, unspecified”. It is a billable ICD-10-CM code that became effective in its current form on October 1, 2025. In medical billing, this code is used to report a diagnosis of leukocytosis or an elevated leukocyte count when the physician has not specified the underlying cause or the specific cell type involved.
Criteria for Using D72.829
You should assign D72.829 only when the following conditions are met:
- Clinical Documentation of Elevation: The medical record explicitly states “leukocytosis,” “elevated WBC,” or “high white count”.
- Lack of Specificity: The physician has not documented a more specific type of elevation, such as neutrophilia or lymphocytosis.
- Absence of a Definitive Underlying Diagnosis: If the leukocytosis is merely a symptom of a more definitive condition already being coded (like acute pneumonia), coding guidelines often prioritize the definitive diagnosis unless the leukocytosis is clinically significant in its own right.
Instructional Notes and Exclusions
Understanding the “Excludes” notes is critical for preventing double-billing or incorrect code combinations.
- Excludes1 (Not Coded Here): This note indicates that certain conditions cannot be coded with D72.829 because they are inherently different or more specific. For example, D72.829 excludes eosinophilia (D72.1) and leukemia (C91-C95). If a patient has eosinophilia, you must use D72.1, not D72.829.
- Excludes2 (Not Included Here): This note means the excluded condition is not part of the current code, but a patient may have both at the same time. D72.829 has an Excludes2 relationship with certain immunity disorders (D80-D89) and neutropenia (D70), meaning both could potentially be coded if they are documented as separate, co-existing issues.
Coding Hierarchy for Elevated WBC Count
To achieve maximum specificity, coders should follow this hierarchy when reviewing a patient’s chart:
| Code | Description | When to Use |
| D72.820 | Lymphocytosis (symptomatic) | Use when documentation specifies an elevated lymphocyte count. |
| D72.821 | Monocytosis (symptomatic) | Use when documentation specifies an elevated monocyte count. |
| D72.823 | Leukemoid reaction | Use for extreme leukocytosis (often >50,000) that mimics leukemia but is due to another cause. |
| D72.825 | Bandemia | Use when there is a documented increase in immature “band” neutrophils. |
| D72.1- | Eosinophilia | Use for elevated eosinophil counts, following the specific sub-codes for IHES or LHES if documented. |
| D72.829 | Elevated WBC, unspecified | Use only when none of the above specificities are documented. |
By strictly following these instructional notes and the hierarchy of specificity, coders can significantly reduce the risk of rejections and ensure the medical record is as accurate as possible.
Common Clinical Scenarios and Examples for D72.829
In a busy clinical environment, leukocytosis often appears as a secondary finding or a “work-in-progress” diagnosis. Because the white blood cell count is a dynamic value that changes rapidly based on the body’s internal state, there are several specific scenarios where D72.829 is the most appropriate choice during the initial phases of care.
The Initial Workup Phase
One of the most frequent uses for D72.829 occurs when a patient presents with vague symptoms such as malaise, fatigue, or a low grade fever. If the initial Complete Blood Count (CBC) shows an elevated WBC count but the physician has not yet identified the cause or the specific cell line involved, D72.829 serves as the definitive placeholder.
For example, a patient arrives at an urgent care center complaining of generalized body aches. The CBC reveals a WBC of 14,500. The physician documents “Leukocytosis of unknown origin, pending further labs.” In this instance, until the results of a differential or a culture are returned and interpreted, D72.829 is the accurate representation of the documented clinical knowledge.
Post-Surgical and Stress-Induced Leukocytosis
It is common for patients to experience a temporary spike in white blood cells following major surgery or significant physical trauma. This is often a physiological stress response rather than a sign of a new infection. If the surgeon notes “postoperative leukocytosis” in the daily progress notes without further specifying it as a neutrophilia or linking it to a specific post-surgical complication like a wound infection, D72.829 is utilized.
Similarly, patients who have experienced a myocardial infarction (heart attack) or severe burns often show an elevated WBC count as part of the body’s acute inflammatory response. When the provider documents this elevation as a separate clinical finding to be monitored, D72.829 captures the condition efficiently.
Medication-Induced Elevations
Certain medications can cause the white blood cell count to rise. The most notable examples are systemic corticosteroids. A patient taking high doses of prednisone for an asthma exacerbation may show an elevated WBC count. If the provider documents “leukocytosis likely secondary to steroid use” but does not provide a specific cell type, D72.829 is the appropriate code to link this finding to the patient’s current medication profile.
Differentiating D72.829 from Related ICD-10 Codes
To maintain a high level of coding integrity, it is essential to distinguish “unspecified” leukocytosis from other hematological findings that may look similar on a lab report but have distinct coding paths.
Getty Images
Leukocytosis vs. Leukemoid Reaction (D72.823)
A leukemoid reaction is an extreme elevation of the white blood cell count, typically exceeding 50,000 cells per microliter. While it mimics the blood picture of leukemia, it is actually a benign (though severe) response to an underlying cause like a massive infection or certain tumors.
- Coding Rule: Never use D72.829 if the physician has explicitly documented a “leukemoid reaction.” You must use D72.823. This distinction is vital because a leukemoid reaction implies a much higher level of clinical complexity and severity than standard leukocytosis.
Leukocytosis vs. Bandemia (D72.825)
Bandemia refers specifically to an increase in “band cells,” which are immature neutrophils. This is often referred to as a “left shift” and is a strong clinical indicator of an acute bacterial infection.
- Coding Rule: If the lab report shows a high number of bands and the physician documents “bandemia” or “left shift,” D72.825 should be used. If the patient has both a high total WBC count and bandemia, check the most recent coding guidelines for sequencing, as bandemia is often considered a more specific indicator of the clinical picture than general leukocytosis.
Leukocytosis vs. Eosinophilia (D72.1)
Eosinophilia is an elevation of a specific type of white blood cell called eosinophils, often seen in allergic reactions or parasitic infections.
- Coding Rule: Because eosinophilia has its own specific category (D72.1), it is excluded from D72.829. Even if the total WBC count is high, if the elevation is driven specifically by eosinophils, you must use the more specific D72.1 series codes.
The Financial and Administrative Impact of Accurate Coding
The choice between an unspecified code like D72.829 and a more specific code is not merely a matter of semantics; it has real-world consequences for the healthcare facility’s revenue cycle and compliance standing.
Claim Denials and Medical Necessity
Payers, including Medicare and private insurers, increasingly use automated systems to screen for “medical necessity.” If a patient is hospitalized for a complex condition but the only codes submitted are unspecified (like D72.829), the payer may question the severity of the case. They may argue that the documented codes do not justify the level of care provided or the length of the hospital stay, leading to partial or full claim denials.
Risk of “Undercoding”
Undercoding occurs when a coder uses a general code like D72.829 even though the medical record contains enough information to support a more specific, higher-weighted code. For example, failing to code “leukemoid reaction” (D72.823) when it is documented can result in the loss of appropriate reimbursement, as more specific codes often carry higher Hierarchical Condition Category (HCC) weights or contribute more significantly to Diagnosis-Related Group (DRG) assignments in inpatient settings.
Audit Scrutiny and Compliance
Frequent use of unspecified codes is often a “red flag” for auditors. Insurance companies and government agencies may view a high volume of D72.829 codes as a sign of poor documentation practices or “lazy” coding. This can trigger a Targeted Probe and Educate (TPE) audit, where the payer reviews a sample of claims to ensure that the documentation actually supports the codes billed. Maintaining high specificity helps shield the practice from these time-consuming and potentially costly reviews.
Best Practices for Clinical Documentation Improvement (CDI)
To move beyond the “unspecified” nature of D72.829, healthcare organizations must focus on Clinical Documentation Improvement (CDI). The goal of CDI is to bridge the gap between clinical findings and the specific language required by the ICD-10-CM manual. When documentation is precise, the code D72.829 is naturally replaced by more specific, high-value codes.
Strategies for Providers to Enhance Specificity
Physicians and advanced practice providers are the primary source of the data used in coding. Small changes in how they document a high white blood cell count can have a massive impact on the final code selection.
- Specify the Cell Line: Instead of simply writing “leukocytosis,” specify the type if a differential is available. For example, “neutrophilia” or “lymphocytosis” provides immediate direction for the coder.
- Link the Finding to a Cause: If the elevation is clearly due to a known factor, such as “leukocytosis due to acute cholecystitis” or “steroid-induced leukocytosis,” documenting that link allows the coder to follow the proper “Code First” or “Use Additional Code” instructions.
- Document Clinical Significance: If the leukocytosis is a minor, expected finding of another condition, note it as such. Conversely, if it is severe enough to require separate monitoring or treatment (such as a hematology consult), that significance should be explicitly stated in the progress notes.
The Power of the Physician Query
When a coder or CDI specialist encounters a record that lists “leukocytosis” but the lab results show something more specific, such as a massive “left shift” or a WBC count of 60,000, they should not simply settle for D72.829. Instead, they should initiate a compliant physician query.
A well-crafted query asks the provider to clarify the diagnosis based on the clinical evidence already present in the chart. For instance: “Based on the WBC count of 55,000 and the presence of immature forms, can the diagnosis of leukocytosis be further specified as a leukemoid reaction?” This proactive approach ensures that the final claim reflects the true complexity of the patient’s care.
Practical Tips for Accurate Leukocytosis Coding
Mastering the nuances of D72.829 requires a blend of clinical knowledge and strict adherence to coding conventions. Use these practical tips to ensure your coding is consistently accurate and compliant.
- Check the “Code First” Notes: Some codes for underlying conditions, such as certain infections or malignancies, include instructions to “code first” the primary disease. In these cases, D72.829 would be a secondary code, if used at all.
- Monitor Annual Updates: ICD-10 codes are updated every year on October 1st. While D72.829 is currently stable, the sub-codes around it (such as those for eosinophilia or specific genetic blood disorders) frequently change. Always use the most current manual or software.
- Correlate with Lab Results: Never code from a lab report alone. A high WBC on a lab printout is not a diagnosis until the physician interprets it and documents it in the record. However, you can use lab results as a prompt to query the doctor for a more specific diagnosis.
- Be Mindful of “Unspecified” Overuse: While D72.829 is a valid code, using it on every chart with a high WBC count can look like “lazy coding” to auditors. Always search the record for evidence of a more specific type of leukocytosis before defaulting to the unspecified code.
Frequently Asked Questions (FAQs)
How do I code transient leukocytosis related to stress or medication if not explicitly documented? If the physician only notes “elevated WBC” and the patient is on steroids or has just undergone surgery, you must code D72.829. You cannot “assume” it is steroid-induced or stress-induced without an explicit statement from the provider linking the two. If the link seems obvious but is missing, a query is the best path forward.
What if the lab shows an elevated WBC, but the physician explicitly states “no clinical leukocytosis”? In this case, you do not code for leukocytosis. The physician’s clinical judgment overrides the raw lab data. They may believe the result is a laboratory error or an insignificant variation for that specific patient.
Can I use D72.829 if the patient has leukemia? Generally, no. If a patient has a confirmed diagnosis of leukemia (C91-C95), the elevated white blood cell count is an inherent part of that malignancy. According to Excludes1 notes, you would code the specific type of leukemia instead of the general leukocytosis code.
Conclusion: Precision in Leukocytosis Coding
Accurate medical coding is the thread that connects clinical care to financial sustainability. While D72.829 (“Elevated white blood cell count, unspecified”) is a necessary tool in the coder’s toolkit, it should be used with precision and caution. The preference should always be to identify and code the most specific manifestation of leukocytosis documented in the medical record.
By focusing on Clinical Documentation Improvement, utilizing the physician query process, and staying diligent with ICD-10-CM instructional notes, healthcare professionals can ensure that their coding is compliant, their reimbursements are fair, and their patient records are a truthful reflection of clinical reality. Precision in coding for leukocytosis is not just about avoiding denials; it is about maintaining the integrity of the healthcare system as a whole.
Expert Tip: Never rely solely on online summaries or cheat sheets. Always consult the official, full ICD-10-CM manual, as it provides the crucial instructional notes, exclusions, and authoritative guidance necessary for truly compliant coding.